by Jeff Stickley | Jan 18, 2016 | Educational Blog
Establishing a fluid barrier between the non-sterile environment and the sterile field is probably the single most-controllable aspect of maintaining good sterile technique. And yet, most veterinary practices incorporate less than adequate barriers by using worn out muslin pack wraps – and storing them on the shelf for months or years – and less than optimal products and techniques in surgery to eliminate the risk of fluid penetration.
The liquid barrier – critical in sterile processing and in the OR – must be maintained in order to prevent microorganisms such as bacteria, fungi and viruses from passing from the environment to sterilized instruments within a pack or through surgical drapes from the patient to the surgical site.
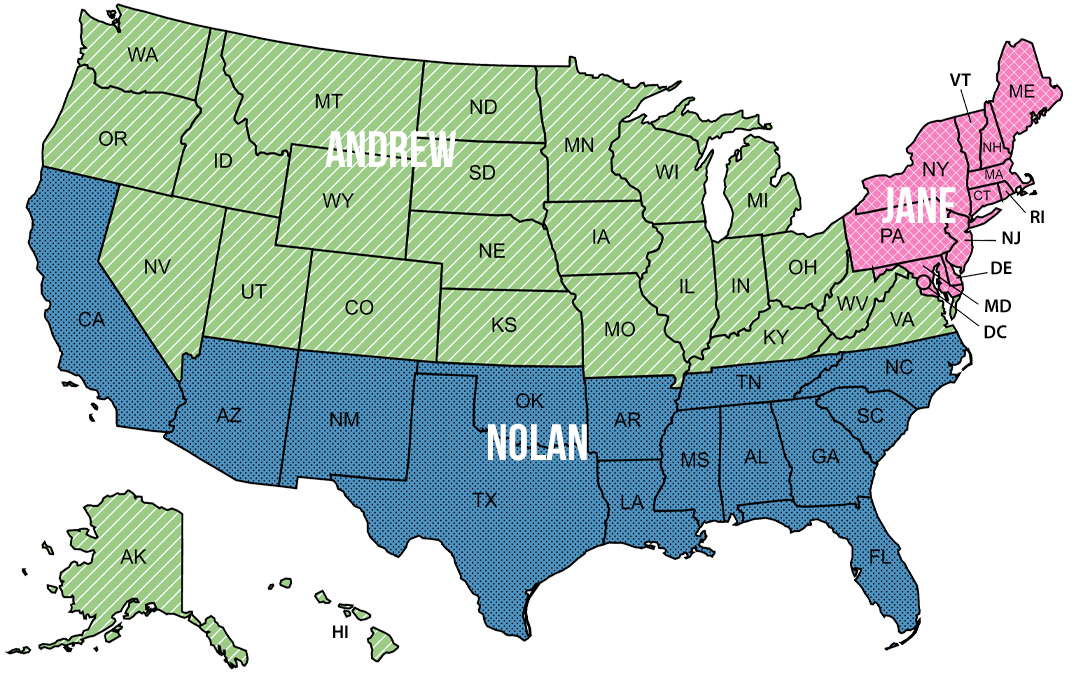
Barrier classifications are established by the Association for the Advancement of Medical Instrumentation (AAMI). The four-level classification system establishes minimum requirements for protective apparel and based on their liquid barrier performance (e.g., efficacy against liquid or liquidborne microorganism penetration). AAMI Standards
In short, if fluid can pass through your drapes, including your instrument tray wrappers, you’re barrier is not up to standard and is a potential source of infection. Every single AHS product, including our innovative, engineered Everlast Sterilization Tray wraps, meets AAMI Level 3 or higher. Do yourself a favor – if you’re going to bother to autoclave instruments, be certain you’re not exposing them to contaminants by using worn out cloth wraps.
What are the AAMI Standards?
AAMI Liquid Barrier Classifications
Level 1 – Gowns and Drapes (the minimum level)
Describes surgical gowns, other protective apparel, surgical drapes, and drape accessories that demonstrate the ability to resist liquid penetration in a laboratory test, AATCC 42 (Water resistance: Impact penetration test).
Level 2 – Gowns and Drapes
Describes surgical gowns, other protective apparel, surgical drapes, and drape accessories that demonstrate the ability to resist liquid penetration in two laboratory tests, AATCC 42 (Water resistance: Impact penetration test) and AATCC 127 (Water resistance: Hydrostatic pressure test).
Level 3 – Gowns and Drapes (minimum for AHS products)
Describes surgical gowns, other protective apparel, surgical drapes, and drape accessories (such as tray wrappers) that demonstrate the ability to resist liquid penetration in two laboratory tests, AATCC 42 (Water resistance: Impact penetration test) and AATCC 127 (Water resistance: Hydrostatic pressure test). For Level 3, the test criterion for AATCC 127 performance is set at a higher value than for Level 2.
Level 4 – Gowns and Drapes (the highest level)
Describes surgical gowns and protective apparel that demonstrate the ability to resist liquid and viral penetration in a laboratory test, ASTM F1671 (Standard test method for resistance of materials used in protective clothing to penetration by blood-borne pathogens using Phi-X174 bacteriophage penetration as a test system). Barriers in surgical drapes and drape accessories also must demonstrate the ability to withstand penetration over a period of time and against the application of pressure, which would help facilitate the fluid transmission through the barrier.
by Jeff Stickley | Jan 15, 2016 | AHS News, Educational Blog
The Problem: Sterilization wrappers with no fluid barrier are of no clinical benefit. If your outer wrap is a muslin or cotton wrap, your technique is not up to standard. Your inner ‘paper’ wrap is only one barrier layer – and that’s not good enough. Every time it’s handled, any number of microorganisms may be passing through this layer to the sterile wrap within!
The Solution: We now offer our Everlast Bleachable Instrument Wraps & Pouches! Want to learn more about this? Check out the Wraps here, and Pouches here.
We are not only moving these faster than we expected, we are getting great feedback, and requests for new sizes!
by Jeff Stickley | Nov 24, 2015 | Educational Blog
Key to establishing the patient component of the sterile field is the surgical draping technique utilized. Most veterinary surgeons have been trained in a simplified draping approach.
Vet Surgery ‘Four Corner Draping’
Generally, veterinary surgical draping utilizes the ‘square-off’, or as humans call it, a ‘universal draping’ technique. This technique is very versatile, and almost any sized drapes can be used on any sized patient. The downside of this technique is excessive material used (wasteful and costly) and – contemporarily – unnecessary tissue trauma to the patient.
How Four Cormer Draping Works
In this manner, four sterile rectangular drapes of roughly the same size are positioned on top of the patient to create an operative ‘window’ in the center. The surgical procedure is performed through this window. Those four drapes are secured to the patient by piercing through them with towel clamps into the patient’s skin (which, though prepped, is considered non-sterile) to ensure they don’t migrate into and contaminate the sterile field. (Tissue trauma created by the towel clamps is considered incidental compared to the risk of the migration of the drapes contaminating the sterile field).
As the sterile barrier has been compromised with the piercing of the first layer of draping by the towel clamps into the non-sterile skin, typical veterinary surgical training often then dictates the application of an additional single, large sterile drape over and above the four ‘square-off’ drapes. This large drape is then fenestrated, the fenestration through which the sterile surgical procedure is then performed.
Improved draping techniques
As in nearly every human surgical procedure in the US, some veterinary surgeries have moved toward a single drape or key sheet draping method. The key sheet, which is often designed specifically for a certain surgical procedure, eliminates the need for all underneath draping – the four-square drapes – and the need to clamp the drapes to the patient skin. These key sheets often incorporate additional performance features (such as less traumatic mechanisms to secure the drape to the patient, tube/cord holders, absorbent material, etc). Using any properly designed key sheet, sterile technique is greatly improved, medical waste is reduced and in most cases, the key sheet is less costly than the 5 drapes it replaces.
Accordingly, Sterile Field Pet Procedure packs are built by draping technique and patient size. Check our options.
by Jeff Stickley | Nov 24, 2015 | Educational Blog
The CDC stipulates that microbial contamination of the surgical site is a necessary precursor to SSI. How might microbes find their way to the surgical site? It turns out, there are a variety of routes in.
Any veterinary surgeon knows that dog fur is resplendent with a variety of bacteria, any of which could be the root cause of an infection.
One way microbes find their way to the site in veterinary surgery is through surgical drapes with an inadequate barrier layer. In order to do their job on the most basic level, a surgical drape must be constructed in such a way as to contain a barrier impervious to fluid penetration. Otherwise, there’s no point in utilizing a drape.
Many surgical drapes, especially muslin/reusable drapes, have lost their barrier nature many, many uses (and many trips through the wash and autoclave) ago. If you’re using old muslin drapes, try a simple permeability test to see if water can simply pass through the drape, which is generally only two layers of muslin.
Many more progressive surgeons have moved to single-use drape materials. Some are better barriers than others. …
by Jeff Stickley | Nov 24, 2015 | Educational Blog
CDC Recommendations for minimizing Surgical Site Infections
Surgical asepsis, attained by Sterile Technique, is the perfect condition for surgery. By definition, this sterile field, if properly and procedurally constructed for each and every surgical patient, means ‘free from microorganisms.’
Such conditions are nearly impossible to attain in human surgical settings but, compared to veterinary surgery, better physical infrastructure, better products and better protocols have been deployed and refined for years to minimize surgical site infections (SSI’s) in human OR’s.
The Centers for Disease Control’s Guideline for the Prevention of Surgical Site Infection, while not specifically written for pet surgery, still offers pertinent recommendations that apply, regardless of the type of animal.
‘Strongly recommended’ steps by CDC to prevent SSI*:
| Step |
CDC Recommendation |
Specific CDC wording |
| Pre-op/Prep |
Do not remove hair unless it will interfere with surgery
|
Do not remove hair preoperatively unless the hair at or around the incision site will interfere with the operation |
| |
Remove hair immediately before surgery |
If hair is removed, remove immediately before the operation, preferably with electric clippers |
| |
Wash and clean around incision site to remove dirt before prepping |
Thoroughly wash and clean at and around the incision site to remove gross contamination before performing antiseptic skin preparation |
| |
Use antiseptic agent for skin prep |
Use an appropriate antiseptic agent for skin preparation |
| Intraoperative |
Wear a surgical mask any and all times in the OR during a procedure |
Wear a surgical mask that fully covers the mouth and nose when entering the operating room if an operation is about to begin or already under way, or if sterile instruments are exposed. Wear the mask throughout the operation |
| |
Cover hair on head and face in OR |
Wear a cap or hood to fully cover hair on the head and face when entering the operating room |
| |
Wear sterile gloves if scrubbed in, after gowning |
Wear sterile gloves if a scrubbed surgical team member. Put on gloves after donning a sterile gown |
| |
Use gowns and drapes that resist fluid penetration when wet |
Use surgical gowns and drapes that are effective barriers when wet (i.e., materials that resist liquid penetration) |
| |
Change clothing that is soiled and/or contaminated with blood and body fluids |
Change scrub suits that are visibly soiled, contaminated, and/or penetrated by blood or other potentially infectious materials |